Difference between revisions of "DuxWare Release Note - 01/19/2020"
Tag: visualeditor |
|||
| Line 17: | Line 17: | ||
Reports>Revenue Analysis>Referring Provider Productivity Report | Reports>Revenue Analysis>Referring Provider Productivity Report | ||
| − | Many of our specialty practices utilize this report to find the top referring providers. | + | Many of our specialty practices utilize this report to find the top referring providers. Prior to this release, this report determined productivity solely from looking at referring providers as they are assigned to a claim. The user can now look at a referring provider's productivity from claims or by referring provider's defaulted in the patient's demographic record. |
| − | Prior to this release, this report determined productivity solely from looking at referring providers as they are assigned to a claim. The user can now look at a referring provider's productivity from claims or by referring provider's defaulted in the patient's demographic record. | + | |
| + | There is a new selection “Referring Provider Source” with two new options available to choose from. | ||
The two options are: | The two options are: | ||
| − | + | * Claim - to include claims based on the referring provider assigned to claims. | |
| − | * Claim | + | * Patient - to include claims based on the default referring provider assigned in the patient's demographic record. |
| − | * Patient | ||
| − | |||
Below is a screen-shot of the criteria page prior to this update: | Below is a screen-shot of the criteria page prior to this update: | ||
| Line 95: | Line 94: | ||
[[File:Batchpost4.png]] | [[File:Batchpost4.png]] | ||
| − | Please see the screen | + | Please see the screen shot provided below to take in all of the tasks that you can perform in one screen. |
Latest revision as of 15:08, 20 January 2020
Reports
Patient Demographics
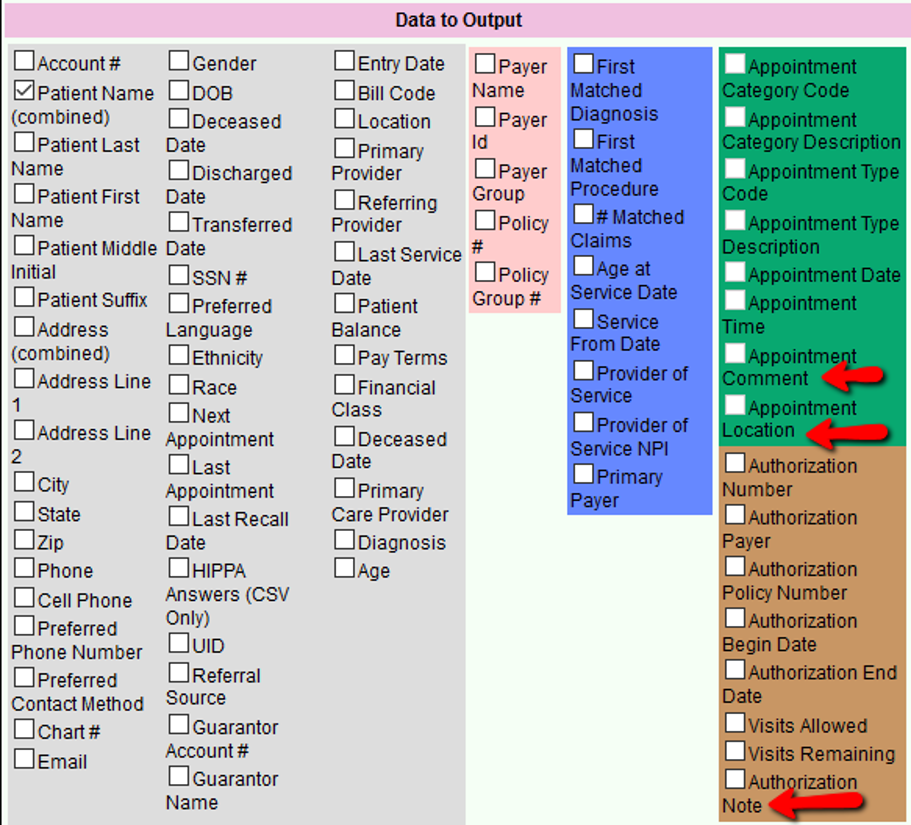
Reports>Patient>Patient Demographics Report.
There are two new output selections for:
- Appointment Comments
- Appointment Location
- Authorization Notes
Revenue Analysis:
Reports>Revenue Analysis>Referring Provider Productivity Report
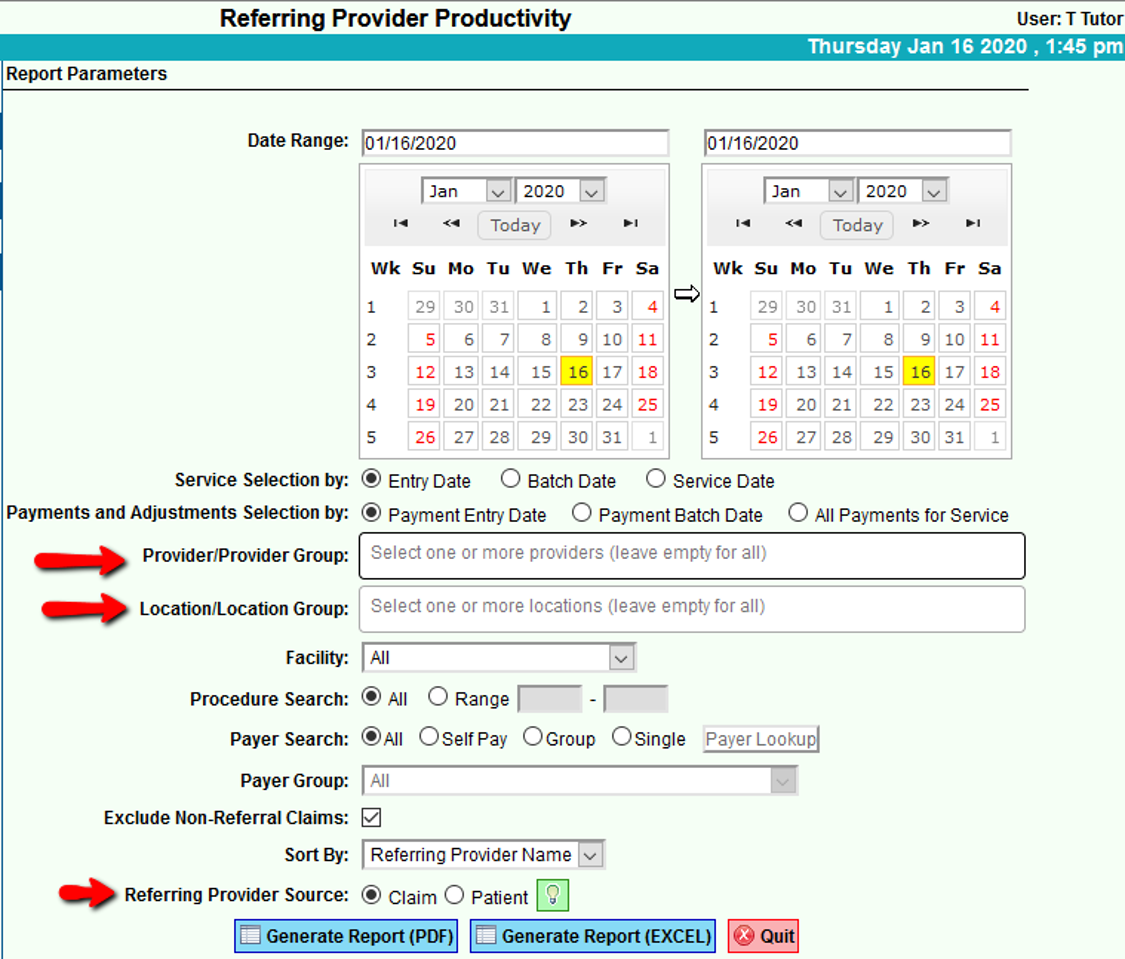
Many of our specialty practices utilize this report to find the top referring providers. Prior to this release, this report determined productivity solely from looking at referring providers as they are assigned to a claim. The user can now look at a referring provider's productivity from claims or by referring provider's defaulted in the patient's demographic record.
There is a new selection “Referring Provider Source” with two new options available to choose from.
The two options are:
- Claim - to include claims based on the referring provider assigned to claims.
- Patient - to include claims based on the default referring provider assigned in the patient's demographic record.
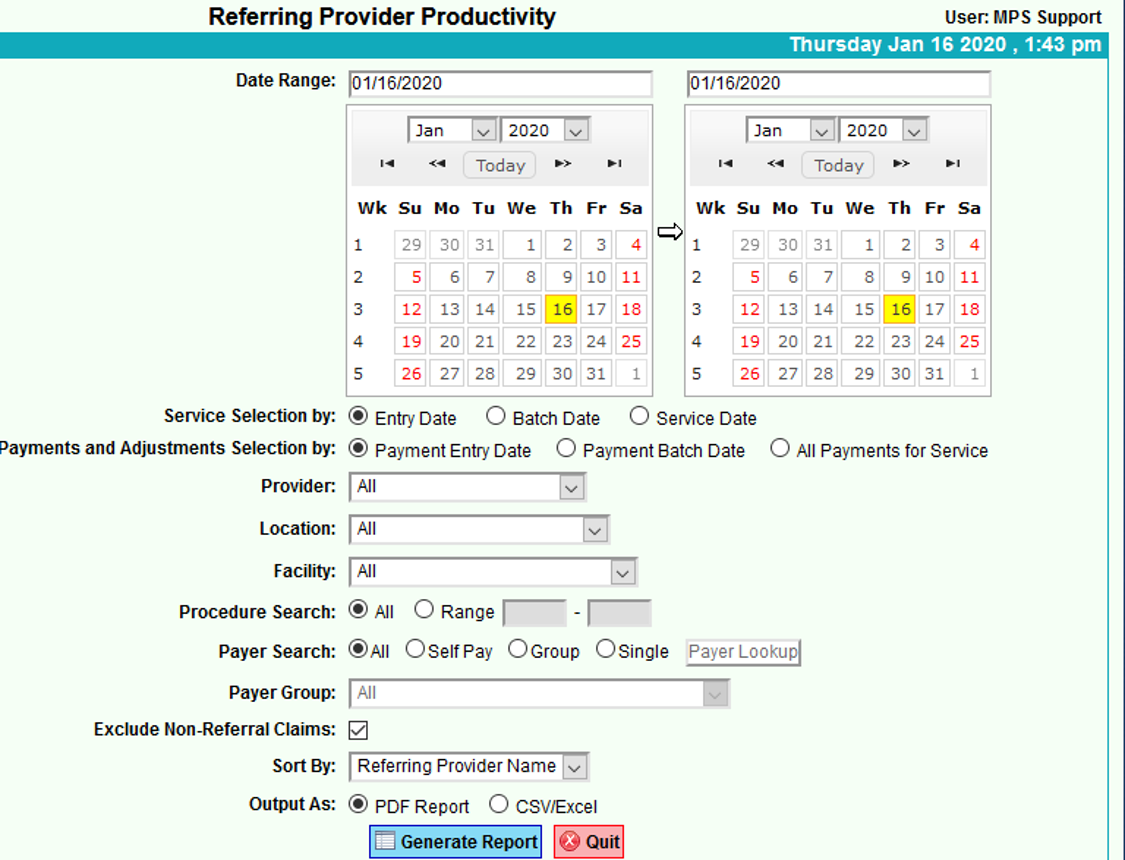
Below is a screen-shot of the criteria page prior to this update:
Updated Referring Provider Productivity Criteria:
Batch Payment Posting
Claims>Batch Posting by Claim #
Modifications have been made to this relatively new feature for Batch Payment Posting. Our users have provided feedback, and we have listened.
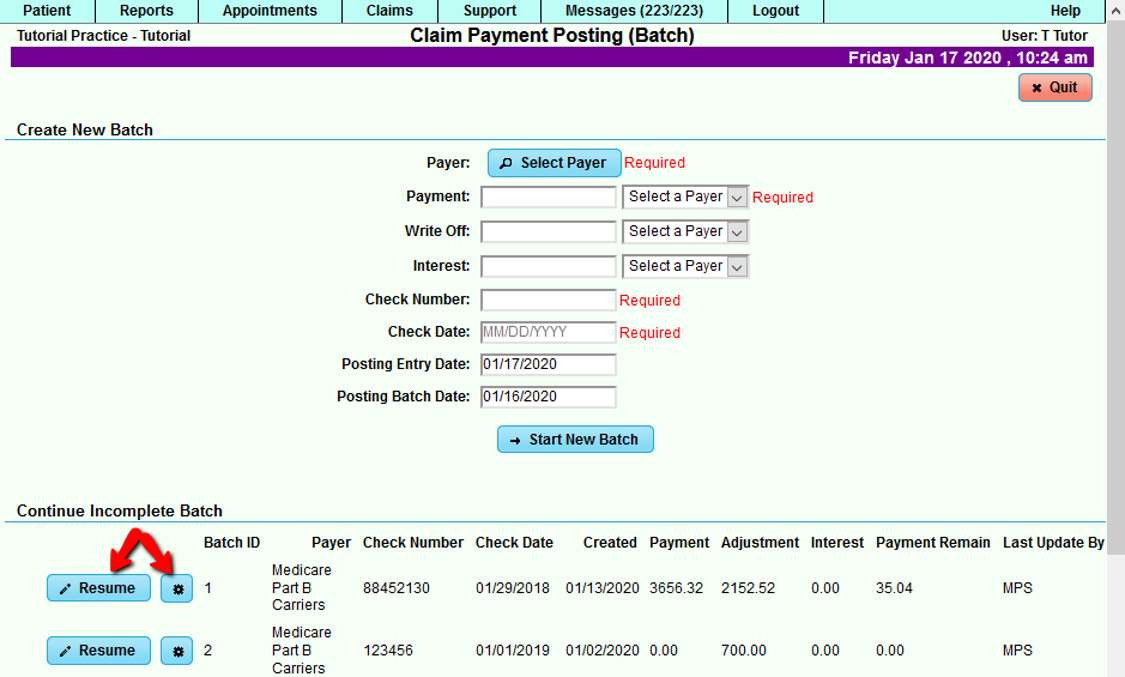
In the Claim Payment Posting (Batch), we have updated the name of the [Continue] button to [Resume], and we have added an option to delete an Incomplete Batch.
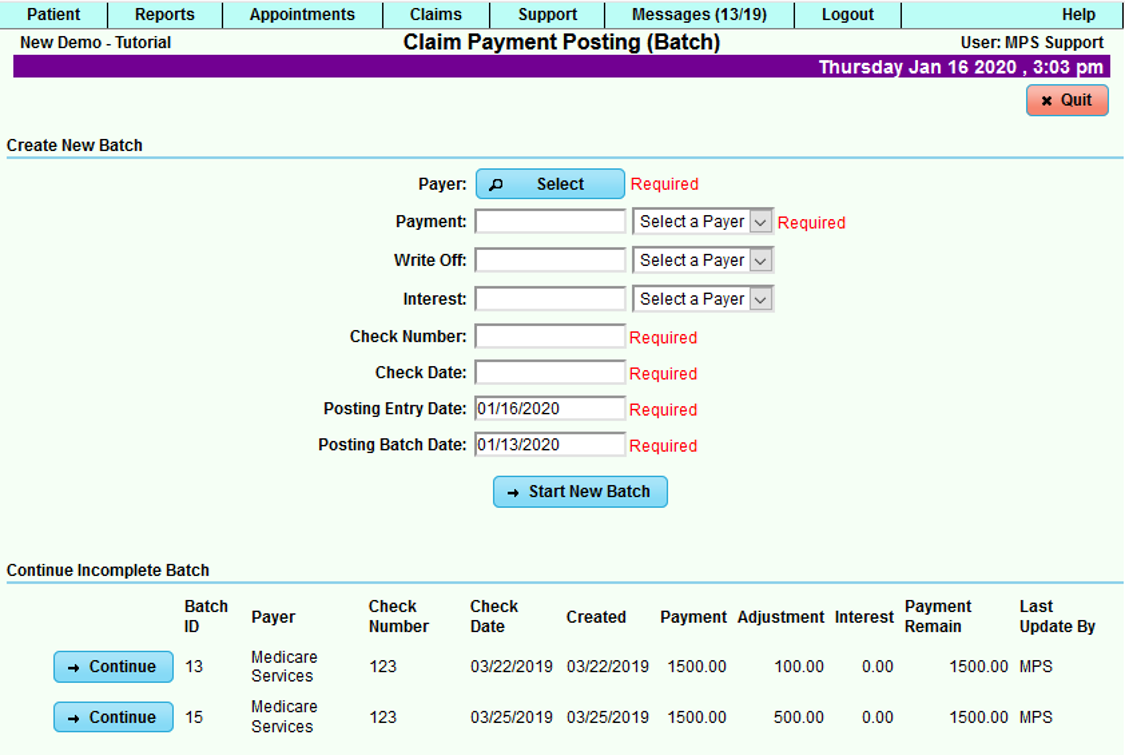
For comparison, the previous page for the Claim Payment Posting (Batch):
Information:
Claim Payment Posting (Batch) allows entry of Bulk EOBs to be input into your Practice Management System for those users who have multiple payments/adjustments to post and have payers that do not send electronic remittances.
You will be able to balance your payments/write-offs to the individual claim and then collectively to the payment/adjustment totals that were input from your EOB before you [Finalize] to post payments/adjustments to claims.
Once claims have posted to a batch, the user has the ability to either leave the batch open to continue/resume posting at a later time, or finalize the batch.
Finalizing the batch will post the payments and adjustments to the claims in the batch.
For multiple adjustments on a single service line, just select the [+] icon to add more adjustments.
To view a history of payment batches, go to Claims tab>Batch Posting Search. If you have posted in previous batches, you will see that either a batch has a status of Finalized or Open. Visit that page for more information.
The updated Claim Payment Posting (Batch) screen below:
You will notice the Create New Batch section is the same, but the Continue Incomplete Batch section has a renamed button and a tool icon.
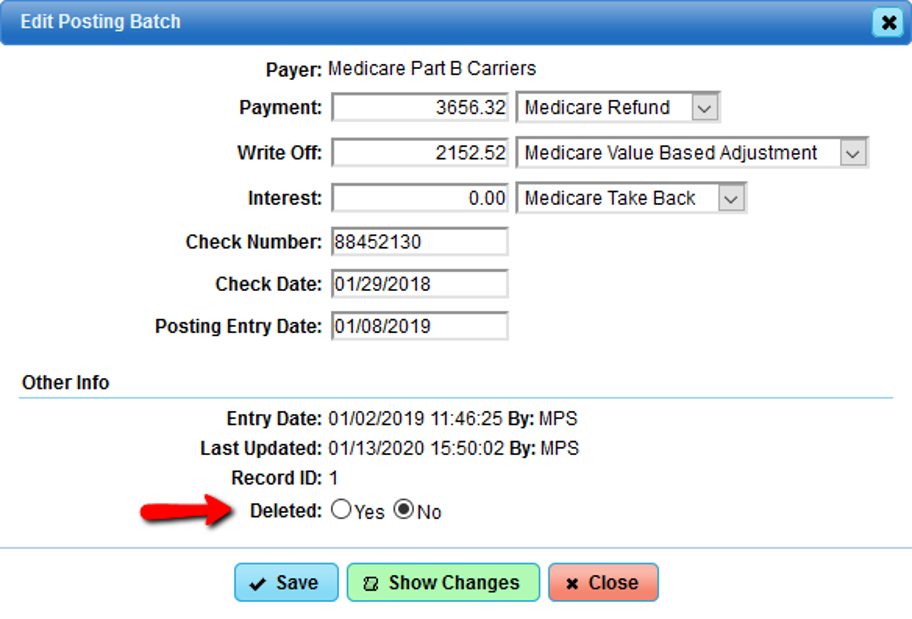
What was the “Continue” button has been renamed “Resume”. The gear icon will allow you to delete the unfinalized batch. This was a very popular request, and now it is available to you.
When deleting an unfinalized batch, keep in mind that nothing was ever posted to the claim/service. In order for the payments and/or adjustments to post, the batch must be “Finalized”.
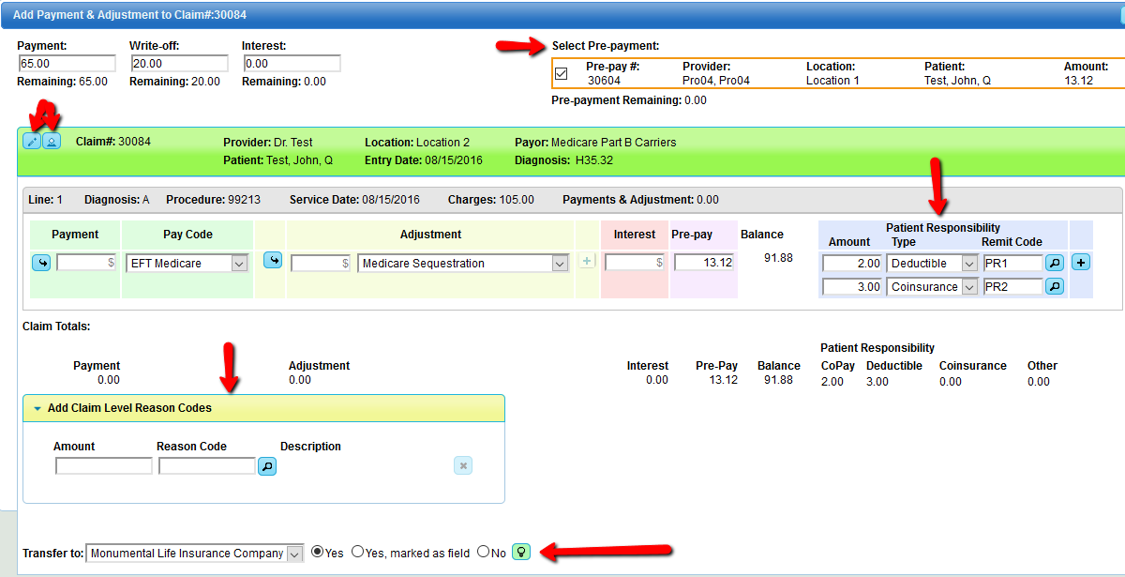
When posting a payment adjustment to the claim, you will now see more added features:
• The ability to select and apply a prepayment • Edit the claim • View Patient • Segregate patient responsible amounts (e.g. PR:1 deductible PR:2 coinsurance) • Add Claim Level Reason Codes • Transfer to next responsible party with options to “Yes”, or “Yes”, marked as filed “No”. o Selecting the option to “Yes, Mark as filed” will transfer to next party as well as mark the next sequence as filed. This is normally done for Medicare cross-over claims, since the primary payer filed the claim electronically for you. o Selecting the option to “NO” will leave the claim on file to the current payer and will not transfer to the next responsible party.
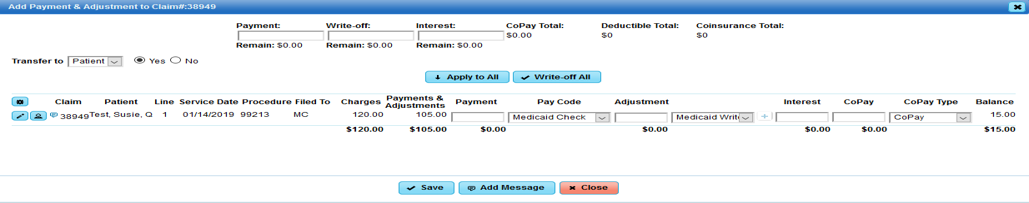
For comparison, below is a screen-shot of the “Add Payment & Adjustment to Claim” page prior this update:
Please see the screen shot provided below to take in all of the tasks that you can perform in one screen.
Batch Posting History:
Claims>Batch Posting History
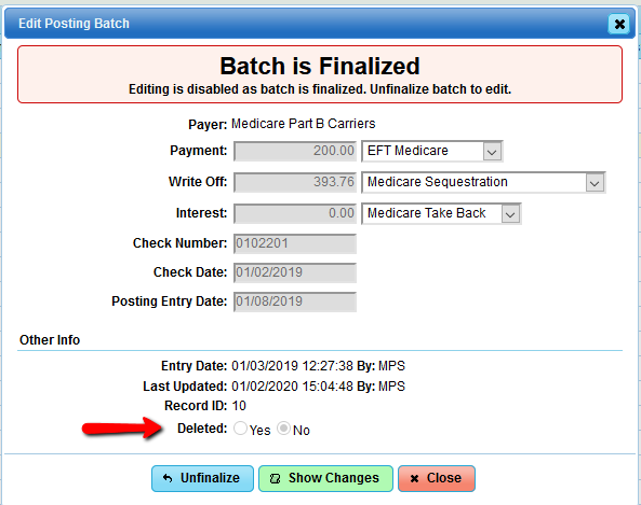
When entering to view a finalized batch, we have added a new dialog box that gives the option to perform a simple delete for that batch. When a batch has been deleted, it will un-post all payments and adjustments that were posted to claims in the respective batch. This works much like the operation of Un-post in our Auto-adjudication batch posting.
If you have any questions or need clarification regarding the items in the PM System updates, please do not hesitate to call or email your PM Support Team. We are always glad to assist you.