Difference between revisions of "DuxWare Release Note - 06/04/2017"
| Line 23: | Line 23: | ||
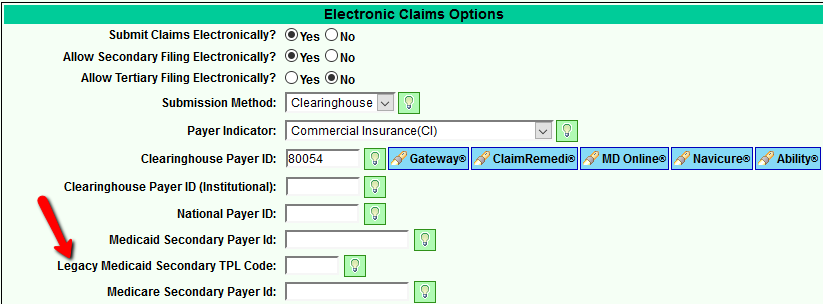
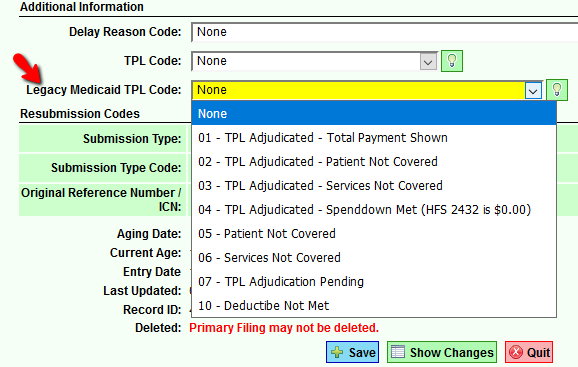
IL Medicaid requires the primary 3-digit TPL legacy code to be submitted with the appropriate 2-digit status code when filing secondary to Medicaid. To accomplish this, the Legacy TPL code for the primary insurance must be obtained from IL Medicaid and input on the Primary policy in the Payer Setup (Support>General>Payer Setup. On the Billing Page, you will input the '''Legacy Medicaid Secondary TPL Code''' in the Electronic Claims Options section. Save your change. If you have a claim that is ready to file secondary to Medicaid, you will then select the appropriate status code for your claim. | IL Medicaid requires the primary 3-digit TPL legacy code to be submitted with the appropriate 2-digit status code when filing secondary to Medicaid. To accomplish this, the Legacy TPL code for the primary insurance must be obtained from IL Medicaid and input on the Primary policy in the Payer Setup (Support>General>Payer Setup. On the Billing Page, you will input the '''Legacy Medicaid Secondary TPL Code''' in the Electronic Claims Options section. Save your change. If you have a claim that is ready to file secondary to Medicaid, you will then select the appropriate status code for your claim. | ||
| + | |||
Excerpt from Billing Options in Payer Setup: | Excerpt from Billing Options in Payer Setup: | ||
[[File:LegacyTPL.png]] | [[File:LegacyTPL.png]] | ||
| + | |||
Excerpt from Claims Filing Sequencing Edit for Medicaid Secondary Filing: | Excerpt from Claims Filing Sequencing Edit for Medicaid Secondary Filing: | ||
| Line 41: | Line 43: | ||
[[File:TertiaryPayerSetup.png]] | [[File:TertiaryPayerSetup.png]] | ||
| − | |||
===Payment Posting=== | ===Payment Posting=== | ||
Latest revision as of 21:50, 4 June 2017
Patient Demographics
Patient Add/Edit:
- Capitalization in Patient Add/Edit has been restored to the original version so that users have the auto-cap as well as the ability to use all caps. (e.g. HWY vs Hwy, US vs. Us).
Configuration:
The following new configuration items have been added to the Configure" section of Patient Add/Edit:
- Require E-mail under Contact info (If no email, instruct your staff to type in the word, "None". If the option is set to "Yes" to require, Patient Add will only accept a valid e-mail such as test@gmail.com or None)
- Include and/or Require Additional Privacy Questions:
- Patient Authorizes the Release of Appointment Time
- Patient Authorizes the Release of Insurance/Billing
- Patient Authorizes the Release of Lab Results
- Patient Authorizes the Release of Medications
Claims Filing
Illinois Medicaid Requirement:
IL Medicaid requires the primary 3-digit TPL legacy code to be submitted with the appropriate 2-digit status code when filing secondary to Medicaid. To accomplish this, the Legacy TPL code for the primary insurance must be obtained from IL Medicaid and input on the Primary policy in the Payer Setup (Support>General>Payer Setup. On the Billing Page, you will input the Legacy Medicaid Secondary TPL Code in the Electronic Claims Options section. Save your change. If you have a claim that is ready to file secondary to Medicaid, you will then select the appropriate status code for your claim.
Excerpt from Billing Options in Payer Setup:
Excerpt from Claims Filing Sequencing Edit for Medicaid Secondary Filing:
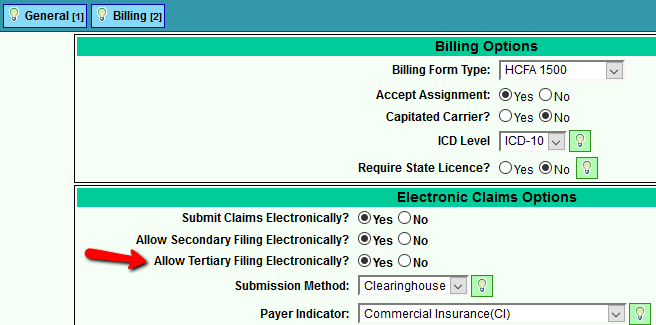
Electronic Tertiary Claims Filing for Professional and Institutional Claims is now available
Review with your clearinghouse to ensure that they accept 837P (HCFA) and/or 837I (UB) tertiary claims. Once you find out if your Clearinghouse and Payer accepts electronic tertiary claims, go to the Payer setup and select "Yes" Allow Tertiary Filing Electronically?. To successfully file tertiary claims, the payment (even if zero) and write-off must be posted to the primary and secondary claim sequences.
Excerpt from Billing Options in Payer Add/Edit:
Payment Posting
Manual Payment Posting:
Users now have the ability to post from any payer that is linked to a claim regardless of the filing sequence. For example, a claim was filed to Medicare. Medicare submits EOB via cross=over to AARP for supplement consideration. Medicare holds their payment, but AARP sends their remittance before the primary payer: Medicare. You now have the ability to simply go in and post your secondary payment without having to manipulate the filing status.